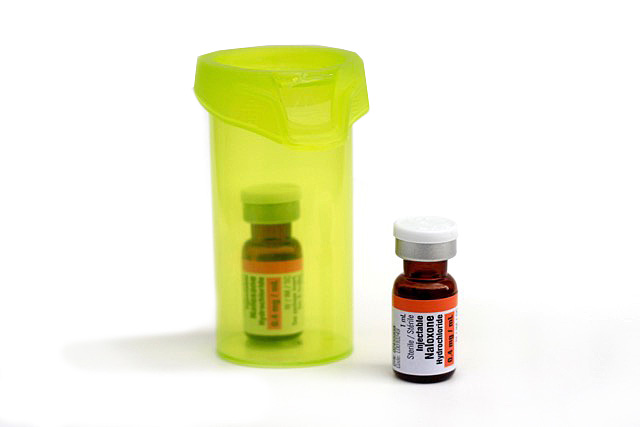
Naloxone Kit
Naloxone is an opioid antidote and can reverse the potentially fatal effects of an overdose. Naloxone is effective against all opioids including: codeine, morphine, hydromorphone (Dilaudid®), meperidine (Demerol®), oxycodone (OxyContin®), fentanyl, heroin, methadone, buprenorphine and others.


Emergency naloxone kits, in both nasal spray and injection formats, are available to ANYONE who may need one at all of our Pharmacies and Clinics. Naloxone kits are available to anyone who is:
- currently using opioids or is a past opioid user who is at risk of returning to opioid use, or
- a family member, friend or other person in a position to assist a person at risk of overdose from opioids.
- How to prevent accidental overdose when using prescription or other opioids
- How to recognize signs of an overdose
- When to use your Emergency Naloxone Kit
- How to use the naloxone nasal spray or intramuscular injection
- The importance of calling 911 and monitoring after naloxone has been provided
- Obtaining a replacement naloxone kit when needed
Preventing an Overdose – Harm Reduction Strategies.
Many harm reduction strategies can be used to reduce the risk of overdose when using an opiate. These include:- Always take prescription opioids as prescribed
- Do not use opioids prescribed for others. Keep your personal prescriptions safely stored where others cannot access (example: in a locked box)
- Do not widely inform others of your opioid prescriptions
- Safely dispose of unused medications at any pharmacy
- Do not combine opiates with other sedatives such as alcohol, benzodiazepines, or other prescription medications
- Take opioids orally instead of smoking or injecting them
- Do not share needles or other instruments
- Always use opioids with another person present and aware of what you are doing
- Keep a naloxone kit on hand in case of accidental opioid overdose
Signs of an Opioid Overdose
Someone may have overdosed if they:- become excessively sleepy, and can’t stay awake, walk or talk
- are not responding to loud voices
- are breathing slowly, shallow, or not at all
- Snoring or groaning when breathing
- Tiny (pinpoint) pupils, or their eyes are rolled back
- Blue or purple lips, nails or skin
- Cold, clammy skin
- Vomiting
How to Respond to an Opioid Overdose Using Your Naloxone Kit
Step 1: Try to arouse the person by shouting their name and shaking their shoulders.Step 2: If the person is unresponsive, always call 9-1-1 first, before administering naloxone.
Step 3: Give Naloxone nasal spray (1 spray into the nostril) or Naloxone injection (inject 1 vial into the arm or leg).
Step 4: Each dose of naloxone can take 2-3 minutes to have an effect. Perform rescue breathing and/or chest compressions (if properly trained) to increase circulation and delivery of oxygen and naloxone to the brain. All kits come with a CPR barrier mask for those who are trained.
Step 5: If there is no improvement after 2-3 minutes, repeat steps 3 & 4. Each kit contains 2 doses of naloxone. Stay with the person until emergency assistance arrives.
If the person begins breathing on their own, or if you have to leave them on their own, put them in the recovery position.

.
Naloxone nasal spray is absorbed through the mucous membrane of the nasal cavity and does not need to be inhaled by the person receiving it. The person should be on their back with their chin pointed upwards to ensure the liquid remains in the nose to be absorbed. Each nasal spray contains one dose only, always use the full dose/spray.
Additional Tips:
Additional Tips:
- Keep the spray in the original packaging until it is ready to use
- Hold your thumb on the bottom of the plunger and the first and middle fingers on either side of the nozzle
- Place the tip of the nozzle into the persons nostril and press firmly, remove from nostril
- Use alternating nostrils for additional doses if required

.
Naloxone works when injected into a muscle; usually the large muscle of the upper arm or upper leg. Choose the most accessible site keeping in mind naloxone can be given through light clothing (but not heavy jackets/jeans).
Additional Tips:
After using your kit, remember to return to your pharmacy to receive a replacement kit as soon as possible.
- Remove the plastic cap from the vial of naloxone
- Draw back 1 ml of air into the syringe
- Insert the syringe into the rubber plug on the vial, and inject the air from the syringe into the vial
- Turn vial upside down and pull back on the syringe plunger to draw 1 mL of liquid into the syringe
- Large amounts of air should be removed from the syringe but small air bubbles can remain
- Insert the needle on a 90-degree angle into the muscle and press plunger to inject naloxone
Naloxone Aftercare
The duration of most opioids is longer than that of naloxone (30-90 minutes) so emergency medical help must always be summoned, even if the person wakes up. With powerful opioid alternatives available, it is possible that more than 2 doses may be required to revive a person. It is also possible that people may require additional doses of naloxone to remain alert once revived. This is why we always contact 911 before administration, to ensure help has arrived before the resources in the emergency kit have run out. Naloxone may precipitate withdrawal symptoms. In most cases, naloxone will only produce mild withdrawal symptoms, however, the benefits outweigh the risks associated with these withdrawal symptoms.After using your kit, remember to return to your pharmacy to receive a replacement kit as soon as possible.

Frequently Asked Questions
A: Yes, anyone taking any opioid is at risk of adverse effects such as decreased respiratory rate. Naloxone can reverse these effects.
A: No, naloxone can save lives if someone else gets access to a person’s opioid and overdoses. Overdoses can happen accidentally in people not using or abusing opioids.
No, naloxone is available in Canada without a prescription.
A: Yes, if a child has overdosed on an opioid, naloxone is the recommended treatment. If the child is not accustomed to having opioids in their body, the naloxone will not cause any withdrawal symptoms.
A: Both! Naloxone nasal spray may be easier for some people to administer, especially if they are uncomfortable with using syringes. Injectable naloxone may work quicker and is a safe and less expensive alternative. If someone has overdosed on an opioid and is in need of naloxone, any kit (nasal, injectable) should be used.
A: In Ontario, naloxone kits are available free of charge for anyone who currently uses, has a history of using, or knows someone who uses opioids (prescription or non-prescription). Kits are also available at no cost for people who may encounter opioid overdose (for example at work, or in their apartment building, community, etc.).
A: Naloxone should be stored at room temperature and protected from light. Avoid storing naloxone kits in a car, where exposure to extreme heat or cold may impact the stability (effectiveness) of the medication. The nasal sprays should be kept in the original packaging. The injectable naloxone should not be pre-loaded into the syringe as this could compromise the sterility and stability of the solution. It is a good idea to inform friends and family members where the kit is stored.
A: The naloxone expiry date can be found on the vials, or nasal spray. You should replace your kit as this date approaches, or if your naloxone becomes discoloured, cloudy or contains particles in the liquid. You should always replace your naloxone kit as soon as possible after use.
A: No, since these are not opioids, naloxone will not be able to reverse the effects. If you are unsure what the person has overdosed on, and they are displaying signs of an opioid overdose, you can still use naloxone. If an opioid was not the cause of the overdose, it will have no effect (neither harm nor benefit).
A: No - Early surveys of opioid users showed they do not use opioids more often if naloxone is available. Naloxone programs also increase the awareness of opioid risks, provide essential education to the public, and help to save lives.
A: No, Ontario health card numbers are used to ensure the pharmacy is reimbursed for the costs of the kit through the Health Network System. However, if you do not have an Ontario health card or do not wish to provide identification when obtaining a naloxone kit, your pharmacist may still provide you with a naloxone kit, free of charge.
A: Your pharmacist simply must ensure you are aware of a few things, including how to identify and respond to a suspected overdose, and how to properly use the kit. If you have already received a kit from someone else, this “refresher” training likely will only take a few minutes.
A: You can receive up to 2 kits at one time. If you use your kits, they expire, or are misplaced, we can provide additional replacement kits. Your healthcare provider will ask you a few quick questions to assess how the kit was used and its effectiveness.
A: Under Canada’s Good Samaritan Drug Overdose Act, overdose witnesses and victims who seek emergency help have some legal protection. The act can provide protection against charges for possessing drugs for your own use, or for violating conditions of your parole, bail, probation or conditional sentence for a simple drug possession charge. An overdose is a medical emergency where seconds count. Please do not delay in calling 911. Additional information can be found, here.






